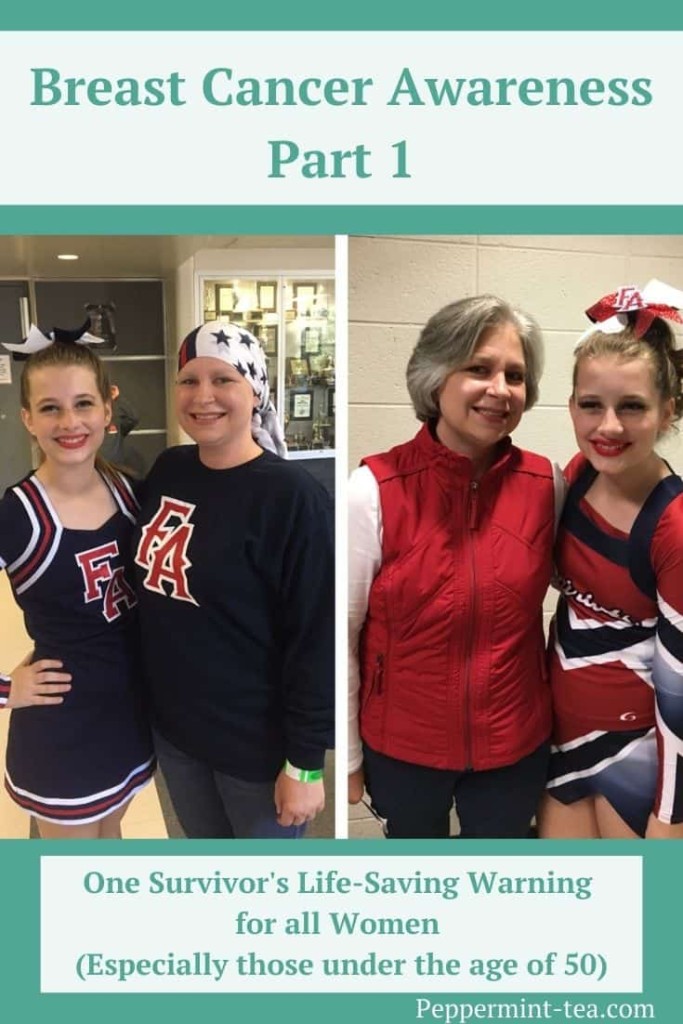
Breast Cancer Awareness Part 1: One Survivor’s Life-Saving Warning to All Women

“You Can Get Breast Cancer When You’re Young”.
October is Breast Cancer Awareness Month, and survivor Susan Leonard has a message for all women. “You can get breast cancer when you’re young.” Susan, unfortunately, knows this from experience. While her warning isn’t meant to needlessly scare others under the age of 50, it is meant to help save lives. After reading this inspiring two-part Q&A with her, I can guarantee that you’ll be motivated to get that mammogram you may have been putting off.
If you don’t know where to start with that or think you can’t afford diagnostic services, there are plenty of resources to get you on your way. After you hear from Susan, I’ll share some of these to guide you in your next steps. Any time of the year is a good time to learn more about breast cancer, but during this month in particular, it’s time to become aware and to take action. I, for one, appreciate Susan’s courage in sharing her story, and I know you will too.
Peppermint Tea & Me: You were diagnosed with breast cancer in March of 2016. How old were you when you were diagnosed?
Susan Leonard: I was 44 years old.
PTM: How was your breast cancer found?
SL: I did find a lump. I had had a mammogram at age 40, like I was supposed to. Then I was supposed to have another one at 42, and I hadn’t had it done. I found a lump, and I ignored it for a little while. I thought this has got to be pre-menopausal something. But it never went away and never changed. I looked at my paperwork and my mammogram was still current, so I just scheduled a routine mammogram. When I told them I had a lump, they said, ‘Okay, we can’t do a routine mammogram, we have to do a diagnostic mammogram.’
PTM: What’s the difference in protocol between a routine and diagnostic mammogram?
SL: I know for the place where I had my mammogram done, when it’s a diagnostic mammogram, they have a doctor onsite who can read it. If additional testing is done, it can be done immediately, and you don’t have to wait. But it’s also a different doctor’s order, and it’s just a whole different procedure. I had to go back to my regular doctor to get the order. They had already scheduled the diagnostic mammogram to happen fairly quickly, but my regular doctor’s office said that I couldn’t be seen for another three weeks. I had to insist that I needed to have the appointment by the mammogram date, and they were able to fit me in.
Note: According to the National Breast Cancer Foundation, a diagnostic mammogram is used after suspicious results on a screening mammogram are found or after some signs of breast cancer such as a lump, breast pain, nipple discharge, thickening of skin on the breast, or changes in the size or shape of the breast alert the physician to check the tissue. “As compared to screening mammograms, diagnostic mammograms provide a more detailed x-ray of the breast using specialized techniques.” They take longer than a screening mammogram because more x-rays are taken that can provide views of the breast from multiple angles.
PTM: What was your life like when you were diagnosed?
SL: David and I were approaching our twentieth wedding anniversary, so we were planning a big trip. Rachel was 15 and was going to be 16 in April. I got my official diagnosis from the doctor on John’s ninth birthday. I was working for a small family-owned company and had been there since 2014 because we were starting to get ready to pay for college. The wife of the owner had actually had breast cancer a few years before I started working there. They were the first people I told other than my immediate family because I knew that I’d have to miss work for testing and other stuff. Since she had been through the whole process, they were very supportive.
PTM: Can you please describe what you were thinking and what you felt when you received your diagnosis?
SL: I was shocked initially because I had no family history. I felt like I was healthy. I didn’t expect to get the diagnosis, but I pretty much knew when they did the mammogram. Since I’d had one at 40, I knew what that one was like. For this one, they took a thousand extra pictures, and then said, ‘Don’t get dressed. Stay right here.’ Then they came back and said they were going to have to do an ultrasound. A doctor has to tell you, but they did say there was definitely a lump there. They weren’t giving me any other options about what it could be, so I pretty much knew from that very first mammogram what I was going to hear. It was still a little shocking and numbing to actually hear it.
PTM: What type of treatment did you go through, and how long did that last?
SL: My cancer was on the left side. I initially had a mastectomy just on the left side. While there were some irregular cells on the right side, there wasn’t any cancer there. The surgeon that I went to for a second opinion wanted me to have an MRI. He said that ‘the type of cancer you have likes to hide and it’s probably more than what you think.’ It did end up being larger, so we decided to do the mastectomy. They said, ‘Let’s just do the left side first and get rid of what we know is cancer. We’ll deal with the right side later.’
So, I initially had a mastectomy on the left side with no expanders, no reconstruction at all. It just left me even less than flat, concave there, and then I did chemo. I was supposed to do 12 rounds of chemo, but I wasn’t able to do the last two rounds because I developed neuropathy in my hands and feet. The doctors felt like the chemo would make it worse so that ended in September of 2016.
PTM: Was that all of the treatment that you had or was there more?
SL: My cancer was 100 percent estrogen positive and 100 percent progesterone positive and then HER2 (human epidermal growth factor receptor 2) negative. As far as cancer goes, that’s a good thing to be. I have to take a hormone blocker and initially got a Zoladex shot, which stops your ovaries from working. After doing that for a year, we decided to go ahead and remove my ovaries and tubes because I was having all of the hot flashes and stuff. I still have to take a pill every day to block the estrogen and will probably do that for 10 years. Then we did the mastectomy on the right side, and I had reconstruction at that time. So that was 10 months later that I had the reconstruction.
The type of cancer that I had was Grade 2 Stage 2b Invasive Lobular Carcinoma, and it likes to migrate to the other side. So that’s why I wanted to have the second mastectomy. You hear a lot of times that once you reach your five-year mark, your chance of recurrence lessens. But with Lobular Cancer it’s the opposite. It usually stays dormant or doesn’t show up again until much later. So that’s why my treatment was a little more aggressive because we were trying to keep it from coming back.
PTM: What were the treatments like, and how did you and your family handle that?
SL: It was really strange. By nature, I am a tearful person. Hallmark commercials make me cry. But when I got the diagnosis, I did not cry. David, the day we got the word, it was John’s birthday, and John was getting ready to come home from school. Someone had called David, and his face was red, and he had been crying. We weren’t going to tell the kids yet. We were going to wait until we knew a little bit more before we told them. And I was like ‘you’ve got to stop. The kids can’t see you like this.’
So initially, I don’t know what happened because that’s just not my personality at all. But when it came to chemo, I was terrified. I’m being treated at Duke University Medical Center, which is a great place to be treated, but they treat so many people that the wait times there are crazy. My very first treatment, I of course had no idea. They did do some pre-chemo training, but you still don’t know what it’s actually going to be like. I did have a port put in in my chest area, so they would just access the port instead of trying to get a vein every time.
Chemotherapy
I’m waiting in the waiting room for chemo to start, and the longer I sit there, I just get more and more anxious, and I’m finally in tears. They finally take me back, and the actual chemo itself wasn’t that bad. The initial chemo I had, the infusion part, lasted maybe three-and-a-half to four hours. I didn’t feel bad until four days later, and then you feel really, really bad. I was taking three different anti-nausea medications and steroids before and after chemo no matter how I felt, so that helped. They also told me when my hair would probably fall out, so I was prepared bookwise, but I wasn’t prepared physically. You just don’t know any of it until it happens.
I didn’t get sick. I never threw up after chemotherapy, but I did develop what they called chemo-anxiety. A couple of times, I threw up before chemo, so they gave me some Ativan to take before my treatments. My worse side effects with chemo were mouth sores and thrush. My blood counts dropped, but usually rebounded pretty quickly. I experienced some nausea, but the medications helped, and I lost all of the hair on my body, including eye brows and lashes.
The good thing about the treatments is that David works at Duke and his office is near the hospital, so he came with me to every single treatment. It’s nice to have an extra set of ears. Because there were times when I’d say, ‘Did the doctor say this?’ and he was like ‘No, they said this.’ So, it was nice to have him there.
Susan’s Story Continues
This was the beginning of Susan’s journey with breast cancer. Find out how she’s doing now, what she’s learned from her experience, the advice she would give to other women and resources to help all women get the testing they need in Breast Cancer Awareness Part 2: One Survivor’s Life-Saving Warning to All Women.






2 Comments